7 Best AI Medical Scribes 2026: Complete Comparison Guide
In today's healthcare landscape, physicians spend an average of 16 minutes on electronic health record (EHR) tasks for every patient they see. This administrative burden not only reduces the time available for patient care but also contributes significantly to physician burnout. AI medical scribes have emerged as a revolutionary solution to this problem, leveraging artificial intelligence to automate the clinical documentation process.
AI medical scribes capture, transcribe, and structure patient-physician conversations into comprehensive clinical notes using natural language processing (NLP) and machine learning. The technology landscape is evolving rapidly, with newer tools incorporating Large Language Models (LLMs) or hybrid approaches that combine traditional NLP reliability with LLMs' advanced contextual understanding. This evolution enables more natural and accurate documentation, allowing healthcare providers to focus on patient care rather than paperwork, ultimately improving both provider satisfaction and patient outcomes.
This comprehensive guide examines the best AI medical scribe solutions available in 2026, comparing their features, capabilities, pricing, and integration options to help you find the perfect tool for your practice.
Here's a quick look at the top AI medical scribes in 2026 before we explore each one in detail:
| AI Medical Scribe | Key Strength | Best For |
|---|---|---|
| DeepScribe | Specialty-specific AI models | Practices requiring highly customized specialty documentation |
| Microsoft Dragon Copilot | Deep EHR integration | Large health systems and hospitals |
| Suki | Fast implementation | Independent practices needing simple setup |
| Notable | End-to-end workflow | Organizations requiring comprehensive automation |
| Augmedix | Flexible service tiers | Facilities wanting human assistance options |
| Freed AI | Affordability | Small clinics with budget constraints |
| Sunoh.ai | Accessible solution | Medical practices wanting contract flexibility |
The Evolution of Medical Documentation

Traditional Documentation Methods and Their Limitations
Traditional medical documentation methods have relied heavily on manual processes, with physicians spending countless hours typing notes, dictating to human scribes, or using template-based systems. These approaches present several challenges:
- Time-consuming: Manual documentation can take up to 6 hours of a physician's day
- Error-prone: Human errors in transcription or data entry can lead to inaccuracies
- Inconsistent: Quality varies based on individual documentation styles and preferences
- Limited scalability: Human scribes are expensive and not always available
The administrative burden of documentation has become one of the leading causes of physician burnout, with studies showing that for every hour spent with patients, physicians spend nearly two hours on documentation and administrative tasks.
The Rise of Human Medical Scribes
To address these challenges, many healthcare organizations turned to human medical scribes—trained professionals who accompany physicians during patient encounters and handle the documentation process. While this solution helped reduce the documentation burden, it also came with drawbacks:
- High costs (typically $15-25 per hour)
- Training and retention challenges
- Inconsistent quality
- Privacy concerns with additional personnel in the exam room
The Transition to AI-Powered Solutions
AI-powered medical scribes represent the next evolution in clinical documentation. These sophisticated tools combine advanced speech recognition, natural language processing, and machine learning to automate the documentation process, offering several advantages over both traditional methods and human scribes:
- Cost-effectiveness: Lower long-term costs compared to human scribes
- Consistency: AI tools maintain consistent documentation quality
- 24/7 availability: No scheduling or staffing concerns
- Continuous improvement: AI systems learn and improve over time
- Seamless integration: Many AI solutions integrate directly with existing EHR systems
Understanding AI Medical Scribes

Core Functionalities
AI medical scribes offer a range of functionalities designed to streamline the documentation process:
- Ambient listening: Capturing patient-physician conversations in real-time
- Transcription: Converting spoken conversations into text
- Natural language understanding: Extracting clinically relevant information
- Note generation: Creating structured clinical notes in standardized formats (e.g., SOAP notes)
- EHR integration: Seamlessly transferring notes to electronic health record systems
Key Technologies Powering Modern AI Medical Scribes
The effectiveness of AI medical scribes relies on several advanced technologies:
-
Natural Language Processing (NLP): Allows the AI to understand and interpret human language, recognizing medical terminology and contextual meaning. Traditional NLP approaches use rule-based systems and statistical models to extract structured information from text, excelling at consistent pattern recognition but sometimes struggling with ambiguity.
-
Large Language Models (LLMs): These newer AI systems bring superior contextual understanding and adaptability to medical documentation. LLMs excel at capturing nuanced medical conversations and maintaining context throughout lengthy patient encounters, though they may require more computational resources than traditional NLP systems.
-
Hybrid Approaches: Many modern AI medical scribe solutions combine traditional NLP's reliability and efficiency with LLMs' contextual understanding and flexibility, creating systems that deliver both consistency and adaptability for clinical documentation.
-
Machine Learning (ML): Enables the system to learn from corrections and improve accuracy over time. ML models can identify patterns in medical conversations and adapt to individual provider documentation styles.
-
Speech Recognition: Converts spoken language into text with high accuracy, even in noisy environments. Advanced systems can distinguish between multiple speakers and different accents, essential for capturing doctor-patient conversations.
-
Clinical NLP: Specialized NLP focused on medical terminology and healthcare contexts, integrating medical knowledge bases and ontologies.
-
Deep Learning: Advanced neural networks that can understand complex patterns and relationships in medical conversations, significantly improving accuracy in specialized medical domains.
Integration with Electronic Health Records (EHRs)
One of the most valuable aspects of AI medical scribes is their ability to integrate with existing EHR systems. This integration can take various forms:
- Direct integration: Native compatibility with EHR platforms like Epic, Cerner, and Allscripts
- API connections: Custom connections to EHR systems through application programming interfaces
- Copy-paste functionality: Generated notes that can be easily transferred to any EHR
- Structured data entry: Mapping note content to specific EHR fields for more advanced integration
The level of EHR integration varies significantly between solutions, with some offering deep integration that automatically populates the appropriate fields, while others provide notes that physicians can easily review and transfer to their EHR system.
Benefits Compared to Traditional Documentation Methods
AI medical scribes offer numerous advantages over traditional documentation methods:
- Time savings: Reduce documentation time by 50-70% on average
- Improved accuracy: AI systems can achieve accuracy rates of 95% or higher
- Enhanced patient experience: More eye contact and engagement during visits
- Reduced burnout: Less time spent on administrative tasks leads to higher job satisfaction
- Better work-life balance: Less "pajama time" spent documenting after hours
- Increased revenue potential: Physicians can see more patients or spend more time with each patient
Key Features to Look for in AI Medical Scribes

When evaluating AI medical scribe solutions, several key features should be considered:
Accuracy and Precision in Medical Terminology
The ability to accurately capture and understand medical terminology is essential. Top AI medical scribes are trained on extensive medical datasets and can recognize:
- Specialty-specific terminology
- Medications and dosages
- Anatomical references
- Diagnostic terms
- Treatment protocols
Traditional NLP-based systems excel at recognizing standard medical terminology and structured data, while LLM-powered solutions often demonstrate superior understanding of context and rare or complex terminology. The best solutions achieve accuracy rates of 95% or higher and continue to improve through machine learning.
EHR Integration Capabilities
Seamless integration with your existing EHR system is crucial for maximizing efficiency. Consider:
- Compatible EHR systems
- Depth of integration (simple copy-paste vs. structured data entry)
- Setup requirements and technical support
- User experience within the EHR workflow
Specialty-Specific Adaptability
Different medical specialties have unique documentation needs. Leading AI scribes offer:
- Specialty-specific templates and workflows
- Customizable note structures
- Recognition of specialty-specific terminology
- Adaptability to various practice types and settings
HIPAA Compliance and Data Security
Patient data security is non-negotiable. Ensure the solution offers:
- End-to-end encryption
- HIPAA compliance certification
- Secure data storage and transmission
- Clear data retention policies
- Business Associate Agreements (BAAs)
Voice Recognition Quality
The foundation of any AI scribe is its ability to accurately capture spoken conversations:
- Multi-speaker recognition capabilities
- Performance in noisy environments
- Accent and dialect adaptation
- Real-time processing capabilities
Workflow Optimization Features
Beyond basic documentation, consider additional workflow features:
- Pre-visit preparation tools
- Post-visit summary generation
- Patient education materials
- Follow-up reminders
- Coding suggestions for billing
Mobile Accessibility
Flexibility in how and where the solution can be used:
- Mobile app availability
- Cross-device synchronization
- Offline functionality
- Cloud-based access
Cost Structure and ROI
The financial aspect is important for sustainable implementation:
- Subscription vs. pay-per-use models
- Hardware requirements
- Implementation and training costs
- Projected return on investment (ROI)
- Contract terms and scalability options
Comparison Table
| Tool | Starting Price | Deployment Model | EHR Integration | Mobile App | Human Review | Specialty Focus | Implementation Time | Free Trial | HIPAA Compliant | Voice Commands | Multilingual Support | AI Technology | Coding Assistance | Note Customization | Key Strength |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DeepScribe | Enterprise pricing | Cloud-based | Epic, Cerner, Athenahealth | Yes | Optional | Multi-specialty with customization | 4-8 weeks | Limited | Yes | Ambient | 25+ languages | Hybrid NLP/LLM | ICD-10 | High | Specialty-specific AI models |
| Microsoft Dragon Copilot | Enterprise pricing | Cloud & on-premise | Epic, Cerner, MEDITECH | Yes | No | Multi-specialty | 4-8 weeks | Limited | Yes (HITRUST) | Ambient | Yes (Spanish+) | Hybrid NLP/LLM | Yes | High | Deep EHR integration |
| Suki | Subscription model | Cloud-based | Major EHRs (Epic, Cerner, Athena, MEDITECH) | Yes | No | 99+ specialties | 1-2 weeks | Yes | Yes | Command & ambient | 81 languages | Hybrid NLP/LLM | ICD-10, HCC | Medium | Fast implementation |
| Notable | $400-600/provider monthly | Cloud-based | Epic, Cerner, Allscripts | Yes | No | Multi-specialty | Extended | By request | Yes | Ambient | Limited | Hybrid NLP/LLM | Limited | Medium | End-to-end workflow |
| Augmedix | Tiered pricing | Cloud & human hybrid | Epic, Cerner, MEDITECH, athenahealth | Yes | Optional (tiered) | 50+ specialties | Varies by tier | No | Yes (HITRUST) | Ambient | 32 languages | Hybrid + human | Yes (CareCues™) | High | Flexible service tiers |
| Freed AI | $99/month | Cloud-based | Copy/paste + direct for some EHRs | Yes (multi-device) | No | Multi-specialty | Minimal | Yes | Yes (SOC 2) | Ambient | Yes | NLP/LLM | Limited | Medium | Affordability |
| Sunoh.ai | $149/month | Cloud-based | EHR agnostic | Yes (iOS, Android) | No | Multi-specialty | Minimal | Yes | Yes | Ambient | English, Spanish, Portuguese, Arabic | NLP/LLM | Limited | Limited | Accessible pricing |
Top AI Medical Scribe Solutions
DeepScribe
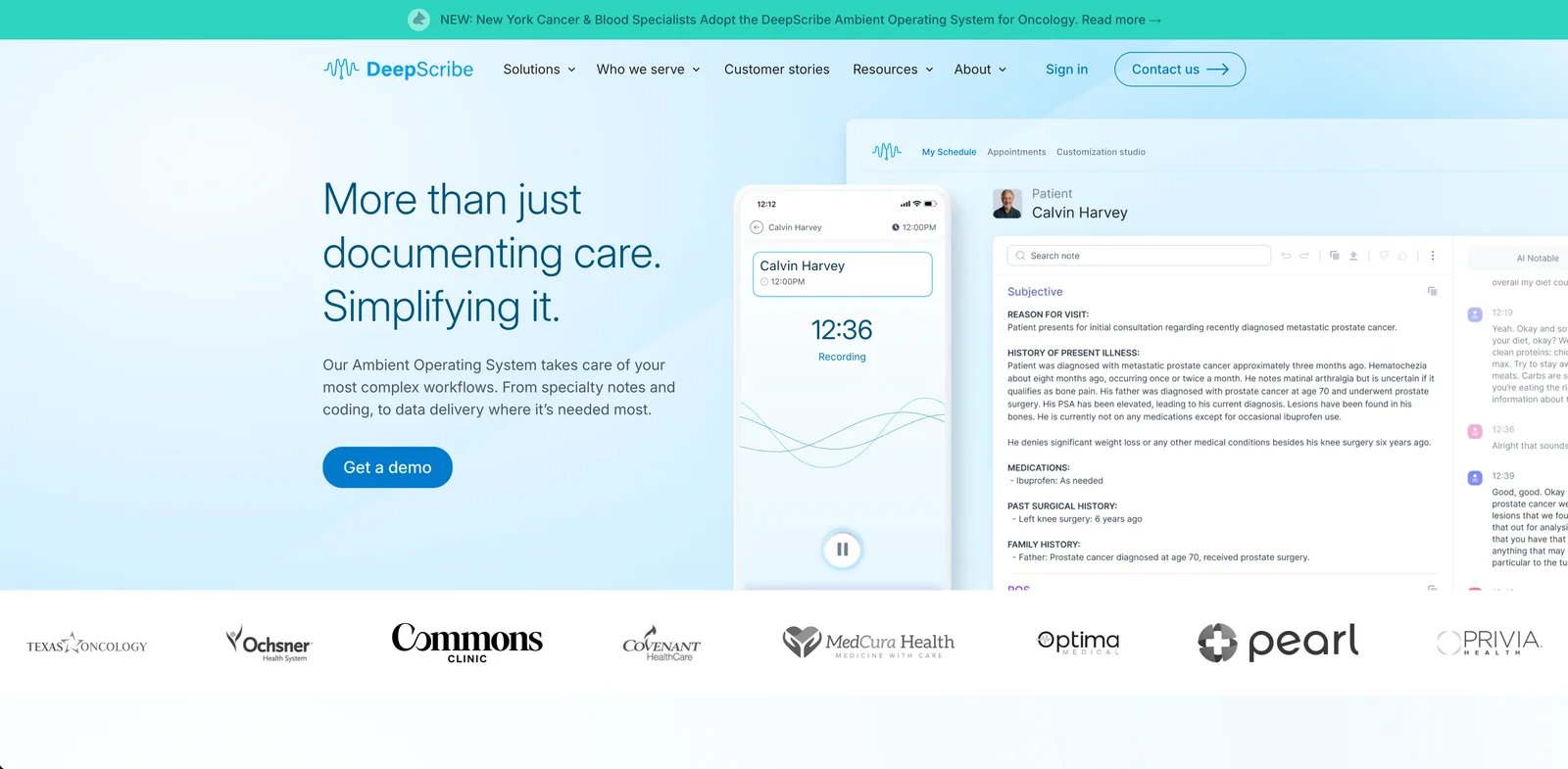
DeepScribe leverages artificial intelligence to automate clinical documentation, allowing healthcare providers to focus more on patient care.
Overview and Company Background
Founded in 2017 by Akilesh Bapu and Matthew Ko, DeepScribe was one of the early pioneers in the AI medical scribe market. The company has secured over $35 million in funding to develop its AI-powered documentation platform and has rapidly grown to become a leading provider of ambient AI scribing technology. Their platform has been trained on more than 5 million patient conversations, creating a robust foundation for accurate clinical documentation.
Key Features and Capabilities
- Ambient AI technology: Captures patient-doctor conversations without requiring specific voice commands
- SOAP note generation: Automatically structures notes in the standard SOAP format with specialty-specific customization
- EHR integration: Seamlessly works with major EHR systems including Epic, Cerner, and Athenahealth
- Multi-specialty support: Customized for various medical specialties with optimized workflows for oncology, cardiology, and orthopedics
- Customization Studio: Offers 50+ options for clinicians to personalize clinical notes according to their preferences
- Multilingual support: Capable of processing conversations in 25+ languages
- ICD-10 coding: Automatically generates relevant diagnostic codes for improved billing accuracy
- Quality assurance: Combines AI automation with built-in verification tools for accuracy
Strengths and Limitations
Strengths:
- High accuracy rates (95.4% overall accuracy according to DeepScore metrics)
- Fast implementation with minimal disruption to clinical workflow
- Continuous learning and improvement based on ongoing user feedback
- Strong user satisfaction ratings (98.8/100 in 2025 KLAS Emerging Company Spotlight Report)
- Specialty-specific AI models for optimal performance in different clinical contexts
- Clinical Moments feature allowing providers to verify the source of any information in notes
- Average 75% reduction in documentation time for physicians
Limitations:
- Premium pricing may be higher than some competitors
- Sales-driven access process that can be cumbersome for smaller practices
- Initial adjustment period required for optimal performance
- More focused on specialty care than primary care documentation
Real-World Performance
According to DeepScribe's internal metrics and third-party verification:
- Average chart closure time of 1.6 minutes
- 59% more accurate documentation compared to GPT-4
- 95.9% major defect-free rate for clinical documentation
- 99.92% note approval rating from physicians
- 75% reduction in total documentation time
Pricing Structure
DeepScribe operates on a subscription model with flexible pricing options:
- Enterprise pricing model based on organization size and implementation needs
- Volume discounts available for larger practices and health systems
- Contact required for personalized pricing information
- Premium pricing reflecting specialized AI models and deep EHR integration capabilities
User Reviews and Third-Party Feedback
DeepScribe has received exceptionally strong reviews in independent evaluations:
- Awarded a 98.8/100 score in the 2025 KLAS Emerging Company Spotlight Report, significantly above industry average
- Received A+ grades across all six evaluation categories: Product, Value, Operations, Relationship, Loyalty, and Culture
- Users consistently report significant time savings and improved work-life balance
- Health systems report high clinician adoption rates (80%+) compared to industry standards
- Physicians highlight improved patient engagement with reduced screen time during visits
As one physician user noted: "I would say my life has changed since adopting DeepScribe. I just feel more relaxed, more chill, not as anxious" (Stacy Jones-Pedescleaux, MD, Family Medicine).
Get started with DeepScribe
Microsoft Dragon Copilot
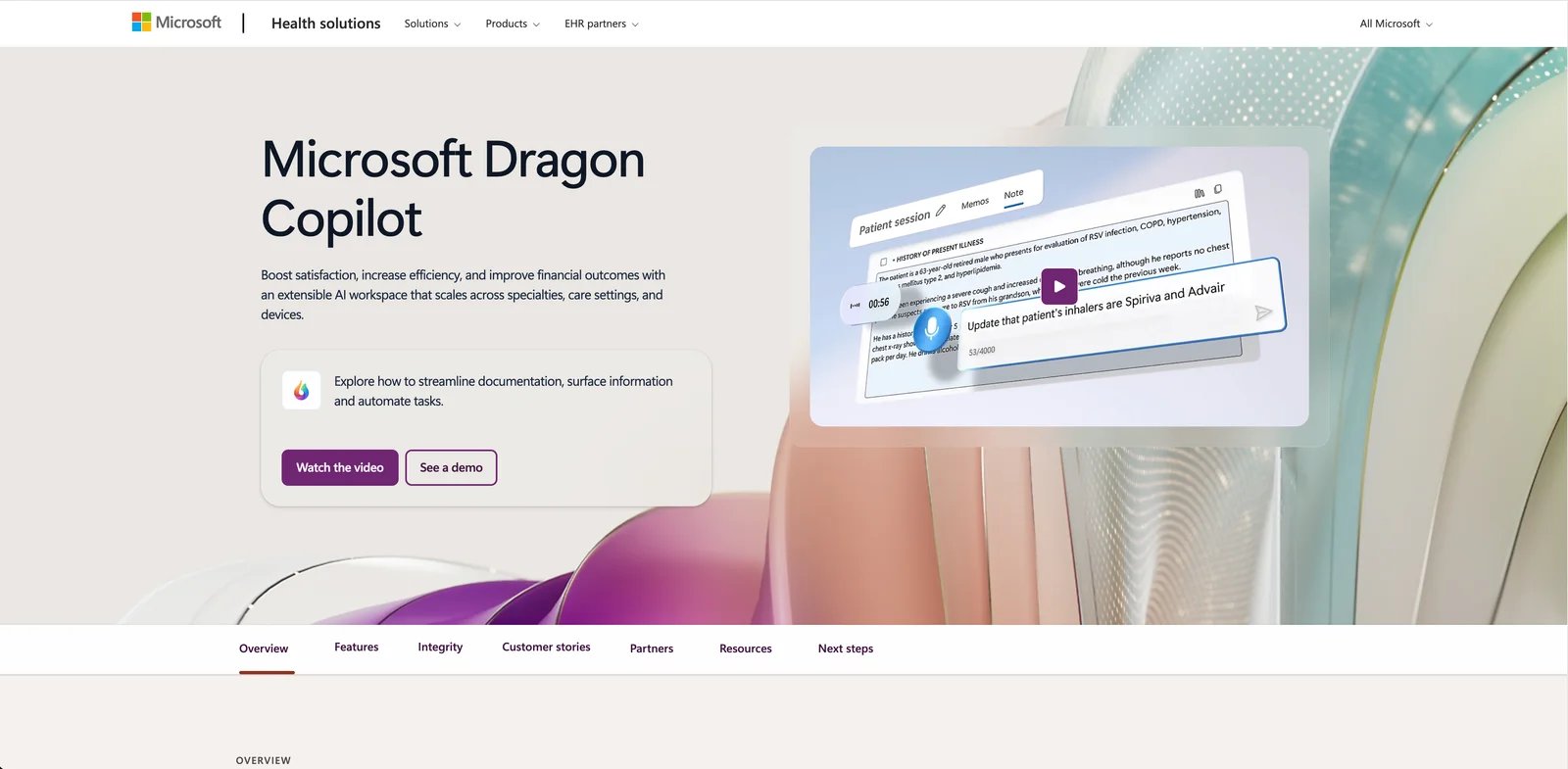
Microsoft Dragon Copilot (formerly Nuance DAX) is a comprehensive AI medical documentation assistant that combines natural language voice dictation and ambient clinical intelligence technology to automatically record and organize patient-physician conversations into accurate clinical notes.
Overview and Company Background
Nuance Communications has been a leader in voice recognition technology for decades, with its Dragon Medical software widely used in healthcare. Microsoft acquired Nuance in 2021 for $19.7 billion and in March 2025 officially launched Microsoft Dragon Copilot, the healthcare industry's first unified voice AI assistant. This solution combines the capabilities of Dragon Medical One (DMO) and Dragon Ambient eXperience (DAX) into a single, integrated platform.
Key Features and Capabilities
- Ambient intelligent listening: Seamlessly captures natural conversations between doctors and patients without requiring specific commands, supporting multilingual communication including Spanish
- Customizable documentation generation: Creates professional clinical notes according to physician preferences in format and style, with options to save templates and AI prompts
- Deep EHR integration: Integrates with major electronic health record systems including Epic, Cerner, and MEDITECH with bi-directional data flow
- Medical information retrieval: Allows clinicians to query note content and obtain reliable medical information with citations from trusted sources
- Comprehensive task automation: Generates conversational orders, referral letters, post-visit summaries, diagnostic evidence summaries, and clinical record digests
- Multi-device support: Offers mobile, web, desktop, and EHR-embedded experiences for seamless cross-device usage
- Note coaching and improvement: Analyzes transcripts and suggests improvements to help capture specific clinical information
Strengths and Limitations
Strengths:
- Built on extensive clinical data from over 15 million patient encounters and billions of minutes of medical dictation
- Enterprise-grade security with HITRUST certification and Microsoft's comprehensive security infrastructure
- Proven time savings of 5 minutes per patient encounter according to Microsoft's survey of 879 clinicians
- Unified platform that eliminates switching between dictation and ambient documentation tools
- Advanced customization options allowing clinicians to tailor notes to their preferences
- Reduced burnout reported by 70% of surveyed clinicians using the technology
Limitations:
- Premium pricing that may be challenging for smaller practices to justify
- Requires specific hardware requirements including iPhone (Android support pending)
- Internet connectivity dependence with potential workflow disruptions during outages
- Initial learning curve to maximize the platform's capabilities
- May require adjustments to existing documentation workflows
- Variable performance across different medical specialties and complex cases
Pricing Structure
Microsoft Dragon Copilot is positioned as a premium enterprise solution:
- Subscription-based licensing model with per-user pricing
- Enterprise implementation packages with optional training and support
- Volume discounts available for larger healthcare systems
- Requires Dragon Medical One Version 2023.3 or later as foundation
- Contact Microsoft or authorized resellers for customized pricing information
User Reviews and Satisfaction
According to Microsoft's surveys and testimonials from healthcare organizations:
- 93% of patients report physicians are more personable and conversational when using the technology
- 62% of clinicians stated they are less likely to leave their organization after implementing the solution
- Healthcare systems like Northwestern Medicine reported a 112% ROI and 3.4% increase in level of service
- Users particularly praise the unified interface that eliminates toggling between different documentation tools
- Hospital executives highlight the security benefits of the Microsoft platform and its enterprise scalability
Healthcare executives from WellSpan Health, Cooper University Health Care, Orlando Health, and University of Michigan Health-West have praised the solution's ability to transform clinical documentation, improve efficiency, enhance security, and ultimately serve as an in-room assistant for patient care.
Get started with Microsoft Dragon Copilot
Suki
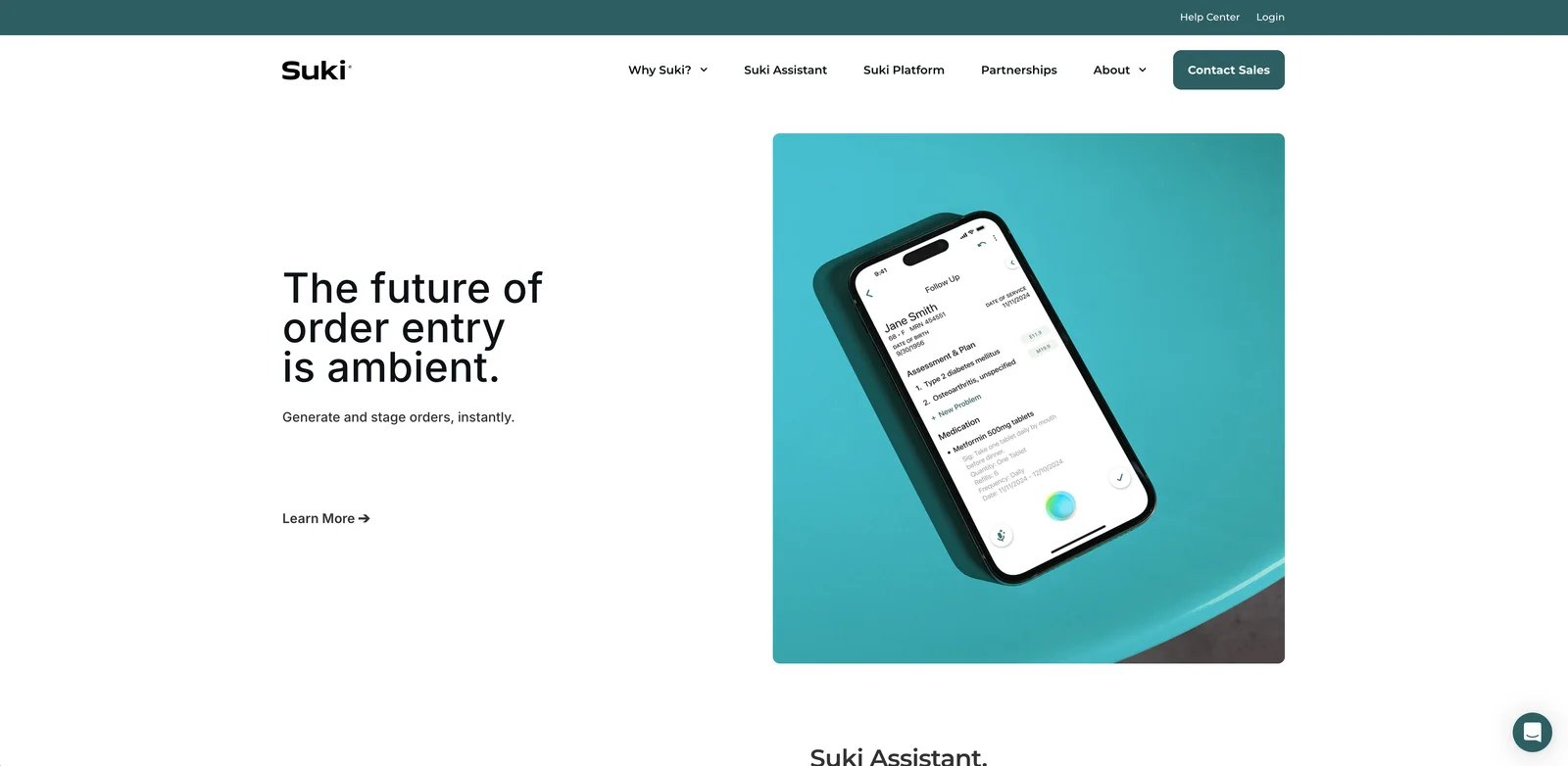
Suki is an AI-powered voice assistant designed specifically for healthcare providers to streamline clinical documentation and reduce administrative burden.
Overview and Company Background
Founded in 2017 by Punit Soni, a former executive at Google and Motorola, Suki was developed to address the documentation burden that contributes significantly to physician burnout. The company has secured substantial funding to build its AI platform and has expanded rapidly across healthcare systems nationwide. Suki's mission is to make healthcare technology invisible and assistive, allowing clinicians to focus more on patient care rather than paperwork.
Key Features and Capabilities
- Ambient documentation: Captures and transcribes patient-physician conversations in real-time, automatically generating structured clinical notes
- Voice-activated commands: Accepts natural language commands like "document physical exam" or "note patient history" to create specific sections of medical documentation
- Ambient order entry: Industry-first feature that allows clinicians to generate and stage prescription orders during conversations
- Deep EHR integration: Offers bidirectional integration with major EHR systems including Epic, Cerner, Athena, and MEDITECH, pulling patient data and pushing completed notes to appropriate sections
- AI coding assistance: Recommends appropriate ICD-10 and HCC codes based on clinical conversations to improve billing accuracy
- Multi-device support: Functions across desktop, mobile, web, and EHR-embedded experiences for flexible workflow
- Multi-specialty capability: Supports clinicians across 99 medical specialties with terminology-specific understanding
- Multilingual support: Handles documentation in 81 languages, enabling service to diverse patient populations
Workflow Integration
- Pre-visit preparation: Accesses patient history and previous documentation from the EHR
- During visits: Actively listens to the clinical conversation, eliminating the need for manual note-taking
- Documentation generation: Creates structured clinical notes in real-time following preferred documentation formats
- Review and verification: Allows clinicians to review, edit, and approve documentation using voice commands
- EHR synchronization: Seamlessly transfers completed documentation to the appropriate EHR sections
Strengths and Limitations
Strengths:
- Reduces documentation time by 72% according to company data
- Offers comprehensive integration with all major EHR systems, unlike competitors with more limited integration
- Maintains consistent documentation structure aligned with clinical best practices
- Shows high adoption rates (70%+) among clinicians due to ease of use and immediate value
- Scales effectively for both small practices and large health systems
- Provides 24/7/365 customer support with minimal IT resources needed from client organizations
Limitations:
- Requires a 2-3 week adaptation period for clinicians to maximize benefits
- May struggle with highly specialized medical terminology in certain subspecialties
- Performance can be affected by significant background noise in clinical environments
- Integration depth varies between different EHR systems
- Training required to optimize voice command efficiency
Pricing Structure
Pricing information is not publicly available, but Suki operates on a subscription model with customized pricing based on organization size and implementation needs.
User Reviews and Satisfaction
According to the 2024 KLAS Emerging Company Spotlight report, Suki earned a high performance score of 93.2/100. Key strengths highlighted by users include:
- Rapid ROI: 95% of organizations would purchase again, with most achieving positive ROI within 60 days
- Efficiency gains: Clinicians complete notes 72% faster, significantly reducing after-hours documentation
- EHR integration: Seamless workflow across major EHR systems including Epic, Cerner, Athena, and Meditech
- Low implementation burden: Successfully deployed with minimal IT resources
- Responsive development: Quickly implements user feedback and feature requests
Common challenges include adapting to specialty-specific terminology, a brief learning curve during initial implementation, and varying integration depth across different EHR platforms.
Healthcare organizations consistently report time savings, improved documentation quality, and enhanced patient interactions as primary benefits.
Get started with Suki
Notable
Notable is an AI-powered automation platform that transforms clinical documentation through intelligent automation, functioning as a comprehensive AI medical scribe solution while also addressing broader healthcare workflow challenges.
Overview and Company Background
Founded in 2017 by Adam Ting, Justin White, and Pranay Kapadia, Notable has positioned itself as a pioneer in intelligent healthcare automation. The company has secured over $100 million in funding and established partnerships with major health systems across the US. Notable's platform combines artificial intelligence, robotic process automation (RPA), and natural language processing to revolutionize the documentation process and administrative workflows.
Key Features and Capabilities
- Ambient voice capture: Records and transcribes patient-physician conversations with high accuracy, eliminating manual note-taking
- Intelligent note generation: Transforms voice recordings into structured clinical documentation that follows specialty-specific formats and provider preferences
- Workflow automation: Integrates the clinical documentation process with pre-visit, visit, and post-visit workflows, creating a seamless documentation experience
- Comprehensive EHR integration: Offers deep integration with major electronic health record systems including Epic, Cerner, and Allscripts, automatically populating notes in appropriate sections
- Intakeless registration: Extends documentation capabilities to include digital pre-visit documentation, reducing administrative burden throughout the entire patient journey
Strengths and Limitations
Strengths:
- Complete end-to-end solution that addresses documentation within the broader patient care workflow
- AI-driven automation that adapts to physician practice patterns and documentation preferences over time
- Deep EHR integration capabilities that reduce data entry redundancy and improve clinical documentation flow
- Advanced analytics dashboard that provides insights into documentation efficiency and quality metrics
- Enterprise-grade security and HIPAA compliance with rigorous data protection measures
Limitations:
- Enterprise-focused solution that may exceed the needs and budget of smaller independent practices
- More extensive implementation process compared to standalone AI scribe solutions
- Higher investment reflecting its broader capabilities beyond basic medical transcription
- May require more substantial technical infrastructure and dedicated IT support
Pricing Structure
Notable utilizes an enterprise pricing model based on organization needs:
- Customized pricing structure determined by organization size and specific implementation requirements
- Typical investment range of $400-600+ per provider monthly for comprehensive implementation
- Additional costs may include implementation support, training, and ongoing technical assistance
- Volume-based discounts available for larger healthcare systems and organizations
User Reviews and Real-World Impact
Notable has garnered positive feedback from healthcare organizations implementing its AI scribe capabilities:
- Healthcare systems report 30-50% reduction in clinical documentation time, allowing physicians to see more patients
- Users highlight improved physician-patient engagement with less time spent looking at screens during encounters
- Organizations note enhanced clinical documentation quality, completeness, and compliance
- Implementation teams praise Notable's customer support and commitment to successful deployment
- Clinical users report reduced after-hours documentation ("pajama time") and improved work-life balance
Get started with Notable
Augmedix
Augmedix offers a suite of AI-powered medical documentation solutions that combine ambient technology with optional human assistance to address various clinical documentation needs.
Overview and Company Background
Founded in 2012, Augmedix pioneered ambient medical documentation in healthcare, initially using Google Glass before evolving its technology platform. The company went public in 2020 and was recently acquired by Commure in a $139 million deal announced in July 2024. Augmedix has generated over 10 million medical notes and partners with major health systems across the US, including HCA Healthcare.
Key Features and Capabilities
- Tiered product offerings: Three distinct solutions (Go, Assist, and Live) with varying levels of AI automation and human support
- Ambient AI documentation: Captures and transcribes patient-physician conversations in real-time across 50+ specialties
- Comprehensive EHR integration: Bi-directional integration with major EHR systems including Epic, Cerner, Meditech, and athenahealth
- Clinical AI engine: Combines automatic speech recognition with natural language processing and specialty-specific fine-tuned large language models
- Multilingual support: Documentation capabilities across 32 languages
- Care gap identification: "CareCues™" feature provides real-time care gap and billing reminders
Strengths and Limitations
Strengths:
- Customizable service levels to match clinical needs and preferences
- HITRUST certified with enterprise-grade security and HIPAA compliance
- Established track record with major health systems, including 4 of the nation's 10 leading health systems
- Specialty-specific solutions including a dedicated app for Emergency Medicine
- Flexible options from pure AI to AI-human hybrid workflows
Limitations:
- Premium pricing for full-service tier with human documentation specialists
- Acquisition by Commure may bring integration and operational changes
- Implementation may require more extensive IT support for some deployment models
- Notable recent declines in stock value prior to acquisition announcement
Pricing Structure
Augmedix offers a tiered pricing model based on service level:
- Augmedix Go: Self-service AI solution with approximately 1 hour of daily EHR time savings
- Augmedix Assist: Hybrid AI-human solution with 1.5-2 hours of daily EHR time savings and signature-ready notes within 1 hour
- Augmedix Live: Full-service solution with dedicated medical documentation specialists offering 2-3 hours of daily EHR time savings
- Enterprise pricing available for health systems with customized implementation packages
User Reviews and Real-World Impact
Augmedix users consistently report:
- Significant time savings allowing for improved work-life balance
- Enhanced patient engagement through better eye contact and attentiveness
- High-quality documentation with reduced administrative burden
- Particular value in high-volume practices and complex specialties
- Positive physician testimony such as "life-changing" and "total game changer" according to customer testimonials
Get started with Augmedix
Freed AI
Freed AI is a cutting-edge AI medical scribe solution designed specifically to streamline clinical documentation and reduce administrative burden for healthcare providers.
Overview and Company Background
Founded in 2020 by Erez Druk, who created the platform after witnessing his physician wife spending countless evening hours completing documentation, Freed AI has quickly gained popularity among clinicians. The company's mission is straightforward: to make clinicians happier by eliminating the burden of after-hours charting. Freed has grown rapidly and is now trusted by over 17,000 clinicians across 650+ healthcare organizations.
Key Features and Capabilities
- Ambient conversation capture: Records and transcribes patient-physician conversations in real-time, generating comprehensive SOAP notes within minutes
- Self-learning technology: Adapts to individual provider styles and preferences through its "Learn this style" feature
- Multi-device compatibility: Works seamlessly across desktop, tablet, and mobile devices
- Multilingual support: Handles documentation across multiple languages
- Simple workflow: Three-step process - capture the visit, edit the note, copy to EHR or use direct integration
- Fast note generation: Produces complete documentation in 1-5 minutes post-visit
- HIPAA-compliant security: Implements robust data protection with SOC 2 certification and HITECH compliance
- EHR integration: Works with all EHRs through copy/paste functionality, with direct integrations available for popular systems like Athena, eClinicalWorks, and Practice Fusion
Advantages and Limitations
Advantages:
- Affordable pricing ($99/month for unlimited visits) compared to competitors and traditional scribes
- No storage of patient recordings, increasing security and privacy
- Minimal training required with an intuitive, user-friendly interface
- Impressive accuracy for medical terminology and medication names
- Ability to learn and adapt to provider's documentation style
- Extensive customer support and onboarding assistance
Limitations:
- May require editing for complex or specialty-specific terminology
- As with all AI scribes, requires review before finalizing documentation
- Voice recognition may occasionally have difficulty with multiple speakers or accents
- Integration depth varies across different EHR systems
User Reviews and Satisfaction
Freed AI has received consistently positive feedback from its user base across various specialties:
- Physicians report saving an average of 2+ hours daily on documentation
- 95% of surveyed users indicate they would recommend Freed to colleagues
- Users consistently praise the accuracy of medical terminology and medication names
- Many clinicians highlight the improvement in work-life balance and reduced burnout
- Positive patient experiences are frequently mentioned, with patients appreciating the increased attention from providers who no longer need to type during visits
Get started with Freed AI
Sunoh.ai
Sunoh.ai is an AI-powered ambient listening technology designed to transform patient-physician conversations into comprehensive clinical notes while streamlining the documentation process for healthcare providers.
Overview and Company Background
Sunoh.ai is a relatively new entrant in the AI medical scribe market, developed by eClinicalWorks, a well-established healthcare technology company. The platform focuses on reducing documentation burden through advanced speech recognition and natural language processing technologies. As of 2025, Sunoh.ai is trusted by over 80,000 healthcare providers across the United States, highlighting its rapid adoption in the medical community.
Key Features and Capabilities
- Ambient conversation capture: Records patient-provider conversations in real-time with support for multiple speakers, accents, and languages
- Multi-language support: Offers documentation capabilities in English, Spanish, Portuguese, and Arabic, with more languages being added regularly
- Multi-device accessibility: Works across various platforms including iPhone, iPad, Android devices, and web browsers
- Clinical document generation: Automatically creates structured SOAP notes and clinical summaries from conversations
- EHR agnostic: Compatible with all major electronic health record systems, though it works alongside rather than deeply integrated in some cases
- Order entry assistance: Captures labs, imaging, procedures, medication orders, and follow-up visit details in the draft notes
- Review and edit capabilities: Allows providers to review, modify, and approve documentation before finalizing
Advantages and Limitations
Advantages:
- Accessible pricing model ($149/month per user) compared to some competitors
- No long-term commitment required
- 24/7/365 customer support included
- Implementation services provided at no additional cost
- Runs on secure Microsoft Azure infrastructure
- Multi-language functionality for diverse patient populations
- High portability across different devices and platforms
Limitations:
- Newer platform with less established track record than some competitors
- EHR integration may be less robust than full-integration solutions
- May require some manual review and editing of generated notes
- Limited customization options compared to more specialized solutions
- Potential learning curve for optimal usage and configuration
User Reviews and Satisfaction
Users consistently report significant benefits from implementing Sunoh.ai:
- Healthcare providers report saving up to two hours daily on documentation
- Users highlight improved work-life balance and reduced burnout
- Many clinicians note that documentation can be completed within two minutes of visit completion
- Practice managers appreciate the improved efficiency, with some reporting a 40-50% reduction in documentation time
- Users praise the system's ability to handle multiple speakers during patient visits
- Customers appreciate the straightforward pricing and absence of long-term contracts
- Multiple testimonials confirm the platform's effectiveness across various specialties and practice sizes
According to user testimonials, Sunoh.ai has proven particularly valuable for busy practices seeking to improve patient interaction while reducing after-hours documentation work, with many providers crediting the tool with helping them "reclaim their pajama time" and complete documentation before leaving the office.
Get started with Sunoh.ai
How to Choose the Right AI Medical Scribe

Finding the optimal AI medical scribe for your practice involves a systematic approach:
Assessment of Organizational Needs
- Current pain points: Identify specific documentation challenges
- Volume considerations: Evaluate documentation load and patient volume
- Integration requirements: Determine must-have connections with existing systems
- Budget constraints: Establish clear financial parameters
- Technical capabilities: Assess your organization's technical readiness
Specialty Considerations
- Terminology requirements: Consider specialty-specific language needs
- Documentation complexity: Evaluate the typical complexity of your notes
- Workflow variations: Assess how your specialty's workflow might affect AI scribe usage
- Regulatory considerations: Address specialty-specific compliance requirements
Budget Planning
- Initial investment: Calculate startup costs including implementation and training
- Ongoing expenses: Project subscription or usage fees
- ROI timeline: Determine when you expect to see financial returns
- Scaling considerations: Plan for potential expansion
Testing and Trial Periods
- Pilot program: Start with a limited implementation
- Evaluation framework: Establish clear success criteria
- Feedback collection: Gather input from all stakeholders
- Performance analysis: Measure against predetermined metrics
- Comparison methodology: If possible, test multiple solutions
Staff Involvement in Selection Process
- Stakeholder identification: Include representatives from all affected groups
- Demonstration opportunities: Provide chances to see solutions in action
- Feedback channels: Create formal ways to collect input
- Champion development: Identify and empower internal advocates
- Consensus building: Work toward shared decision-making
FAQ
What is the average time savings when using an AI medical scribe?
Are AI medical scribes HIPAA compliant?
Can AI medical scribes work with all EHR systems?
How accurate are AI medical scribes compared to human scribes?
What specialties benefit most from AI medical scribes?
What is the typical ROI timeframe for implementing an AI medical scribe?
Which AI technology is better for medical transcription: traditional NLP or LLMs?
Traditional NLP systems excel at targeted, rule-based tasks with structured data extraction and consistent pattern recognition. They typically offer:
- Higher reliability for standardized medical terminology and well-defined workflows
- More computationally efficient processing for time-sensitive applications
- More controlled, explainable processing paths, which can be important for regulatory compliance
- Consistent performance in handling specific clinical tasks with lower error rates for common scenarios
LLM-powered solutions provide greater contextual understanding and flexibility. They demonstrate:
- Superior ability to handle ambiguity and interpret nuanced medical conversations
- Better adaptation to novel situations and rare terminology
- Greater capability to maintain context over lengthy documents
- Improved performance with complex, non-standard phrasing
Many leading AI medical scribes now employ hybrid approaches, combining traditional NLP's reliability and efficiency with LLMs' contextual understanding. When evaluating solutions, consider the complexity of your medical specialty, documentation needs, and whether standardization or flexibility is more critical for your practice.
How do AI medical scribes handle complex medical terminology?
Can AI medical scribes be customized for specific clinical workflows?
How do different AI technologies compare in medical transcription accuracy?
Discover More AI Tools
Explore our comprehensive directory of AI tools, carefully curated and reviewed by experts to help you find the perfect solution for your needs.